| |
April
2015
- Volume 9, Issue 2
Transcultural Adaptation of Best Practice Guidelines for Ostomy
Care: Pointers & Pitfalls

|
 ( (
|
Samar Ali
Abdul Qader
Mary Lou King
Correspondence:
Samar Ali Abdul
Qader
University of Calgary
Qatar
Email: samar16164@gmail.com
|
 |
|
Abstract
Objective: No standardized guidelines for ostomy
care exist in the Middle East to support best practice.
This contrasts with North America where ostomy guidelines
are widely used in health service organizations. It
is unknown whether guidelines developed in one country
are relevant to other parts of the world. This project
sought to assess the relevance of North American ostomy
guidelines to a different health system and cultural
context in the Middle East. The overall aim was to reach
consensus to adopt, adapt or reject.
Methods: A graduate student, enrolled in a Masters
of Nursing (MN) program in the Gulf Cooperation Council
(GCC) state of Qatar, critiqued two North American guidelines
using standardized tools. The process engaged local
stakeholders and opinion leaders in the colorectal cancer
field, as well as international ostomy care and practice
guideline experts.
Results: Results of this critique, combined with
input from internal and external stakeholders, resulted
in a hybrid guideline that has been used in a Muslim
society with different demographic, health system and
cultural contexts.
Conclusions: Appraising the quality, content
and relevance of international ostomy guidelines to
different jurisdictions provided the opportunity for
local practitioners to define and shape best practice.
The adapted guideline is expected to promote consistent
standards of care and optimal health outcomes for persons
with ostomy in a region where cultural and religious
values are intricately linked to health beliefs and
practices.
Key words: Practice Guidelines; Adaptation; North
America; Middle East; Ostomy Care.
|
1. Introduction
International data indicate that colorectal cancer is the
third most common malignancy in the world, with 1.4 million
new cases diagnosed in 2012 [1]. In the Middle East, the incidence
of colorectal cancer is < 10 per 100,000 population; this
is substantially lower than North America, Australia and New
Zealand [2]. However, higher rates have recently been reported
in Israel and Qatar, where age standardized rates range from
30-40 per 100,000 population [1,2]. This is consistent with
findings of a study conducted in Qatar at the turn of the
century identifying that colorectal cancer rates in this small
Arabian Gulf country were higher than other Gulf Cooperation
Council (GCC) states, with the most common sites being the
sigmoid and descending colon [3]. Despite advancements in
oncology surgery in the past decade, ostomy formation remains
one of the major treatments for colorectal cancer [4]. As
such, stoma formation surgeries are on the rise around the
world concurrent with the increase in colorectal cancer.
An ostomy is an opening (stoma) from inside the small or large
bowel to the outside [5]. Ostomy can be permanent, when an
organ (the small intestine, colon, rectum, or bladder) must
be removed. It can be temporary, when the organ needs time
to recover. The most common ostomies are a colostomy, ileostomy
and a urostomy.
Patients with ostomy have physical, nutritional, spiritual,
health education and psychological support needs. It is important
for nurses, physicians and other health care providers to
understand the comprehensive needs of patients who have undergone
ostomy so they can provide responsive care. The goal of health
care providers is to assist patients with ostomies to achieve
optimal independence, self-care abilities, nutritional health
and bio-psycho-social-spiritual well-being. There is a trend
to standardize care and management approaches around the world
using clinical guidelines. The goal is to promote optimal
outcomes and reduce practice variation [6].
Clinical guidelines are systematically developed recommendations
to support provider and patient decisions about health practices
to achieve high quality care [6]. A facility and literature
review undertaken by a graduate nursing student in the GCC
state of Qatar revealed that no practice guidelines relevant
to ostomy care were in use in the Middle East. Furthermore,
no studies could be found that evaluated ostomy care of patients
with stomas in this part of the world.
Guideline adaptation is the systematic approach used to customize
an existing guideline to suit the local context; it is an
alternative to guideline development [7]. Decisions affecting
the adaption, adoption or rejection of guidelines are influenced
by several variables. These include the quality of the guideline,
the scientific evidence supporting the guideline, clinical
expertise, patient preferences, policies, culture and budget
[8]. Authors of the Abu Dhabi Declaration cite four reasons
that practice guidelines developed in one part of the world
cannot simply be adopted in other regions. They include: (1)
differences in culture, genetics, and environmental factors;
(2) variations in patients' presenting features and stage
of disease; (3) differences in health service access such
as technology or drugs; (4) evidence supporting the guidelines
may be generated from populations or contexts with limited
relevance to other jurisdictions [9]. A notable advantage
of adapting existing guidelines is to reduce duplication of
effort, while allowing health providers to integrate local
perspectives into the guideline content [10].
2. Methods
2.1 Purpose
Critiquing North American ostomy guidelines and assessing
their relevance to a different geographic and cultural context
was the focus of this student-led graduate project. The process
engaged local stakeholders and opinion leaders in the colorectal
cancer field, as well as international ostomy care and practice
guideline experts. The aim was to appraise the potential use
of guidelines developed in North America in the local context
and to reach consensus to adopt, adapt or reject. Engaging
Middle East health professionals in guideline appraisal enabled
clinical leaders to assert their critical thinking skills
and give input regarding the "fit" with the local
health system and the cultural-spiritual beliefs and values
of the population.
The following questions served as the focus of inquiry:
1. What practice guidelines currently exist in ostomy care
and management to support best practice of nurses and other
health care professionals?
2. What are the strengths and weaknesses of existing ostomy
care guidelines?
3. What is the relevance of the ostomy care guidelines to
the Qatar health care system and population?
2.2 Philosophical Underpinnings
This work was philosophically grounded in the principles of
evidence-based practice (EBP) which involves the explicit
use of the current best evidence to make decisions about patient
care [11]. It involves augmenting health care providers' clinical
expertise with quality research data. Evidence-based nursing
(EBN), a subset of EBP, is the application of relevant, valid
evidence to inform clinical decisions, with consideration
of clinical expertise, patient preferences and conditions,
available resources, as well as the judgment and qualifications
of the nurse [12]. Besides the widely held view that EBP leads
to high quality care and the best patient outcomes [9], experts
assert that EBP also reduces practice variations, promotes
consistency of care, enhances patient safety, increases self-care
capacity and improves provider satisfaction [13,14]. At a
system and organizational level, EBP has been shown to improve
cost-effectiveness [15].
2.3 Methodological Framework
The CAN-Implement adaptation and implementation planning resource
version-3 was the overarching framework used to critique and
assess the relevance of the two North American ostomy guidelines,
to the Middle East [7]. This comprehensive framework comprises
3 phases: (1) problem identification; (2) solution building
and (3) implementation, evaluation & sustainability. It
is structured around 9 sequential steps, each designed to
assist users to evaluate, adapt and implement guidelines at
the point-of-care. Each step consists of specific activities
associated with the evaluation of existing practice guidelines
and includes strategies for making decisions about their relevance
to local contexts (Figure 1).
Figure 1: CAN-Implement Guideline Adaptation and Implementation
Planning Resource
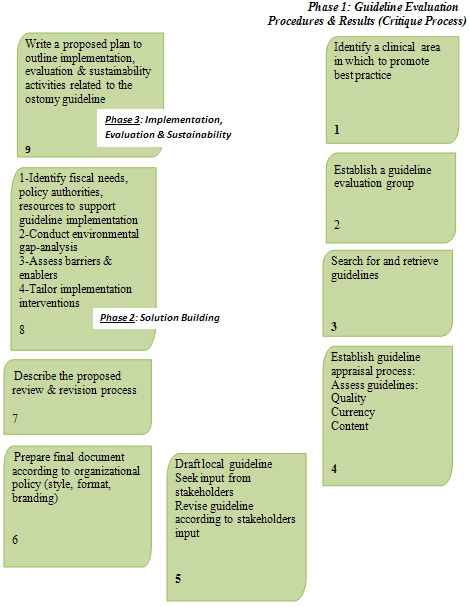 Adapted
from Harrison, M. & van den Hoek, J. (2012). Canadian
Guideline Adaptation Study Group. CAN-IMPLEMENT: A Guideline
Adaptation and Implementation Planning Resource. Queen's University
School of Nursing and Canadian Partnership Against Cancer,
Kingston, Ontario, Canada. Adapted
from Harrison, M. & van den Hoek, J. (2012). Canadian
Guideline Adaptation Study Group. CAN-IMPLEMENT: A Guideline
Adaptation and Implementation Planning Resource. Queen's University
School of Nursing and Canadian Partnership Against Cancer,
Kingston, Ontario, Canada.
2.3.1 Critiquing Process -- CAN-Implement Phase 1
Phase 1 of the CAN-Implement framework consists of 7 steps.
The initial four steps involve the following activities: (1)
identifying a clinical best practice target; (2) establishing
an interprofessional team who will participate in the evaluation;
(3) describing the strategies to locate existing guidelines;
and (4) clarifying the processes, as well as criteria for
appraising the guidelines. Activities of steps 5-7 entail
seeking input from stakeholders and/or opinion leaders, drafting
a document to reflect the consensus of evaluation team members
and outlining the plan for on-going reviews and revision processes.
These final 2 steps focus on: (1) identifying policies, stakeholders,
resources and an implementation plan and (2) assessing the
clinical environment for barriers and facilitators that may
influence guideline use, specifying implementation interventions,
as well as evaluation and sustainability strategies.
3. Results of Phase 1 Critique
3.1 Practice Guideline Target
As noted in the introduction, no practice guidelines for ostomy
care are currently in use in the Arabian Gulf region. To reduce
practice variation and to ensure optimal standards of care
and patient outcomes, a practice guideline was deemed necessary.
The largest health care corporation serving the major population
of Qatar was the target site for this project. In 2013, over
50 new stoma surgeries were performed at this large tertiary
care center.
3.2 Guideline Evaluation Group Formed
Led by the graduate nursing student, a guideline evaluation
group was formed. The team consisted of the student's academic
supervisor as well as clinical experts, including the physician
lead for colorectal cancer services and two advanced clinical
nurse specialists (ANCSs) in the GI program.
3.3 International Ostomy Care Guidelines Located
A literature search uncovered a Canadian ostomy care and management
guideline published by the Registered Nurses Association of
Ontario (RNAO) [16] and an American practice guideline for
fecal ostomy developed by the Wound, Ostomy and Continence
Nurses Society (WOCN) [17]. From the Association of coloproctology
of Great Britain and Ireland (ACPGBI) and the Scottish Intercollegiate
Guidelines Network (SIGN), sixteen colorectal guidelines were
found; however, none were relevant to stoma care or management.
Scrutiny of other data bases, including the World Health Organization
(WHO) Guidelines, National Institute for Clinical Excellence
(NICE) Clinical Guidelines, National Cancer Care Network (NCCN),
Royal College of Nursing, Cumulative Index to Nursing &
Allied Health (CINAHL), Pub Med and Google Scholar, resulted
in no guidelines related to ostomy care. The two guidelines
from RNAO and WOCN were the focus of critique in this project.
3.4 Guideline Appraisal Process Established
3.4.1 Instruments
Literature indicates the Appraisal of Guidelines for Research
and Evaluation (AGREE II) instrument is the universally recognized
gold standard for evaluating practice guidelines [18]. The
AGREE II tool has been translated into 32 languages and is
employed widely to assess the quality of guidelines. The World
Health Organization, the Council of Europe and the Guidelines
International Network recommend this tool for guideline appraisal.
The AGREE II instrument consists of 23 Likert scale items
grouped into six domains. These include: scope and purpose,
stakeholder involvement, rigor of development, clarity and
presentation, applicability, and editorial independence [19].
Domain scores are influenced by the degree to which the guideline
development processes are described and the strategies used
to reach agreement about recommendations for practice [20].
Besides generating separate quality scores in each domain,
the AGREE II instrument enables the appraiser to assign an
overall quality rating of the guideline. This global score
indicates whether the guideline is accepted for use in practice
(e.g. adopted without modification, adopted with alteration(s)
or not adopted). Field testing of the AGREE instrument has
shown acceptable internal consistency (Cronbach's alpha .64
to .88) [19].
An additional tool, the Rapid Critical Appraisal (RCA) Checklist
for Evidence-Based Clinical Practice Guidelines [21] was also
used in the guideline review process. Scoring criteria for
this 17-item checklist are grouped into three quality domains:
credibility, applicability and generalizability. Two items
unique to this brief checklist addressed practice relevance
which had not been covered in the AGREE II instrument. As
such it offered an enhancement to the AGREE II tool. No publications
reporting validity/reliability testing of the RCA tool could
be found.
Consultation with the primary author at Ohio State University
in USA confirmed the tool has not undergone psychometric testing
(email communication B. Melynk, Dec. 13, 2014).
3.4.2 First Level Critique
An independent appraisal of each guideline using the two standardized
tools was completed by the graduate nursing student. This
was followed by an inter-rater reliability check by the academic
supervisor. Revisions were made and results of this first-level
analysis were then shared with the two ACNSs on the evaluation
team. Rather than completing a comprehensive independent critique,
ACNSs reviewed the initial critique, offered recommendations
about the guideline quality, relevance and content and gave
input about resources and ostomy care issues specific to Qatar.
3.4.3 Second Level Critique
In the ensuing 2nd level analysis, data from the individual
critique of RNAO and WOCN guidelines were synthesized by the
graduate nursing student and used to inform the recommendation
to adopt or adapt elements of one or both guidelines. Strengths
and weaknesses of each guideline were appraised specific to
content, relevance and quality. A composite summary was created
structured around the domains of AGREE II tool [18].
3.5 Recommendation to Adapt Guideline
Adopting a guideline means accepting all of its content, including
recommendations [22]. However, if all of the content or recommendations
in the guideline are not considered relevant to local contexts,
the evaluation team selects information considered applicable
and reformats it into a new guideline. This is the process
of adapting guidelines [22]. Following review and appraisal
of both RNAO and WOCN guidelines, a recommendation was made
to adopt with revision (adapt), the RNAO best practice guideline
(BPG) on ostomy care and management and to adopt select parts
of the WOCN guideline.
3.6 Local Guideline Drafted
Following the comprehensive review and critique of the Canadian
and American guidelines [16, 17], the graduate student, acting
as project lead, recommended adaptation of the RNAO guideline
with additions from the WOCN guideline for use in Qatar. The
revised guideline included 19 of 26 recommendations from the
RNAO guideline and the pre-operative ostomy education component
from the WOCN.
3.7 Input from Internal Stakeholders Obtained
As recommended by the CAN-implement authors [7], the adapted
BPG was presented to internal stakeholders on the guideline
evaluation team for their input and approval. Besides obtaining
the perspective of the two ACNSs and senior colorectal-oncology
surgeon, advice from clinical pharmacologists was sought.
Pharmacists suggested including the generic name, along with
the medication category, in the medication flow sheet to ensure
patient understanding. Other suggestions included: (1) eliminating
sensitive information from the sexual information sheet to
avoid cultural inappropriateness; (2) presenting nutritional
management tips in user-friendly language to ensure information
is understandable to users; and (3) translating the patient
information sheets to local languages to be useful to consumers.
3.8 Guideline Revised According to Stakeholder Input
Feedback from internal stakeholders was incorporated into
the final guideline adaptation. Final approval to proceed
with the implementation of the proposed guideline into local
practice was received from the clinical lead of colorectal
services and ACNSs.
3.9 Final Document Prepared According to Policy
Preparing the final document for internal use in local contexts
required consideration of style, format and branding issues
to ensure a standardized appearance with other practice guidelines
(BPGs) in the organization.
3.10 Review and Revision Process of Local Guideline Specified
Organizational policy and procedure specific to each health
care centre will inform decisions about revision processes.
For instance, the organization targeted for ostomy BPG implementation
requires that guidelines be reviewed every three years or
earlier if new evidence is published, a problem is identified
or there is a change in operational, administrative or clinical
practice. The graduate student (now employed as an ACNS in
the organization), will regularly monitor internal, local,
regional and international practices. She will also be on
the lookout for new clinical practice guidelines, systematic
reviews and randomized controlled trials pertaining to ostomy
care and management. Continuing consultation with internal
and external experts in ostomy and colorectal cancer care
will be essential to ensure the most current evidence from
new studies, grey literature and/or unpublished trials is
considered in guideline revisions [10].
4. Discussion
4.1 Ostomy Guideline Implementation in the GCC Health System
Context
Having completed the phase 1 critique of two international
guidelines, the next steps in the CAN-Implement model, namely,
phase 2 solution building and phase 3 implementation, evaluation
and sustainability, require attention to local contextual
variables that influence use of the adapted guideline. Priority
activities focus on assessing the organizational and cultural
context into which the guideline will be introduced.
4.1.1 Organizational Challenges and Opportunities
Careful analysis of organizational policies, stakeholder involvement
and resource implications need to be considered before guideline
implementation and evaluation can proceed. At the health care
corporation in Qatar targeted for guideline implementation,
policy approval must be obtained from the quality management
department and corporate policy chapter committees (CPCCs).
Final decision-making authority regarding the introduction
of any proposed guideline (whether new or revised) resides
with these bodies. Following signed approval of the CPCC lead
officer, the proposed guideline is then submitted to the regulatory,
accreditation and compliance services (RACS). At this level,
a corporate memo is generated confirming the guideline meets
standardized criteria. It is then forwarded to the Chief Executive
Officer of the organization where final sanction is obtained
before posting on the hospital intranet. These policies are
intended to ensure consistent practice regarding guideline
approval processes in the organization.
The involvement of clinical experts, opinion leaders and relevant
internal stakeholders is critical in all phases of the guideline
implementation and evaluation process. Input and expert knowledge
of two clinical nurse specialists, two clinical pharmacists
and a surgeon from the colorectal team helped to ensure guideline
content and implementation - evaluation plans were realistic
and practical. External personnel with expert knowledge of
ostomy care and implementation science were identified who
could provide problem-solving assistance or consultative guidance
as required. Throughout this initiative, liaison occurred
between the graduate nursing student and international experts
whose resource materials had guided each stage of the project
[7, 16, 17].
A budgetary plan specifying implementation and evaluation
expenses is integral to any guideline project. This will require
consideration of production, distribution, marketing, education
and evaluation costs. To promote fiscal responsibility, existing
human resources in the organization were identified to support
the implementation and evaluation of the adapted ostomy guideline.
For instance, nurse educators will be involved in teaching
staff on the two surgical floors, surgical intensive care
unit (SICU) and operating theatre where most of the ostomy
care is provided. The initial training will be delivered in
a four-hour intensive workshop. Staffing needs in these units
may need to be temporarily increased until the education of
all nurses is complete. An evidence-based practice champion
(EBPC) on each unit will be identified, who possesses excellent
interpersonal skills and knowledge competencies specific to
ostomy care. EBPCs will attend a one-day intensive workshop
to prepare them to act as unit-based resources. This "train-the-trainer"
approach [23] is intended to promote effective resource utilization,
as well as staff engagement in the change process. The graduate
student (now ACNS) will act as resource to EBPCs who are assuming
a leadership and mentoring role in supporting the implementation
of the ostomy guideline at the unit level. Recognition and
feedback to EBPCs is deemed important at this early stage
of guideline implementation as it represents the movement
towards a culture of evidence-based practice.
4.1.2 Gap Analysis
After policy, stakeholder and resource issues have been considered,
experts suggest an internal gap analysis be conducted to clarify
what and how much needs to be changed in existing practices
and systems to support effective guideline implementation
[7]. A gap analysis involves assessing the degree of congruence
between current ostomy care practices and guideline recommendations.
Practice variations related to ostomy care uncovered in the
analysis will inform planning decisions regarding practice
change, educational content, implementation strategies and
timelines. On the other hand, current ostomy practices that
are consistent with the guideline will be the focus of positive
feedback.
In the preliminary gap analysis, the project lead noted that
nurses working in the four units treating patients with stoma
do not all have knowledge of ostomy risk factors and peristomal
complications. This will become part of the educational content
during the guideline training. The gap analysis also uncovered
variance between current professional practice and recommendations
related to colostomy irrigation and use of suppositories.
This content will also be incorporated into the guideline
training.
Besides identifying professional practice variance, an organizational
gap analysis may also uncover deficiencies related to resources
and/or health system capacity. For example, a resource issue
apparent in this project was related to the heavy workload
of the two ACNSs in the GI and colorectal cancer program.
Both provide the ostomy care support in the organization and
both have similar roles to that of Enterostomal Therapy Nurses
(ETNs). Their role begins pre-operatively and continues throughout
the post-operative and follow-up phase of the patient's care
trajectory. A future consideration may be to delegate ostomy
care to the wound care team or to hire certified ETNs. Whoever
performs the role of ostomy specialist assumes responsibility
for ensuring high standards of ostomy care through consultation,
education, collaboration and team coordination in order to
promote consistency and continuity of care amongst all multidiscipline
staff.
With respect to health system capacity, limited information
is available about the role of home care services in Qatar
related to the post-discharge needs of new ostomy patients.
This gap, related to care continuity following hospitalization,
represents an important area for further exploration and improvement.
As the change process evolves, it will be important to identify
facilitators and enablers likely to foster implementation
success. Understanding barriers will enable the team to plan
effective strategies to address obstacles that might interfere
with effective implementation. Recognizing facilitators will
provide insight about the forces likely to result in successful
implementation [7]. The implementation strategy for the ostomy
care and management guideline for local use will be informed
by data obtained from the steps previously described. That
is, input from project advisors, budgetary planning, resource
availability and unit-based gap analysis, as well as barriers
and enablers will shape implementation decisions.
4.1.3 Evaluation/Monitoring
Evaluating the effective use of new guidelines requires consideration
of organizational capacity, resource needs and monitoring
strategies. To assess the outcomes of the ostomy guideline
implementation in the Qatar health care corporation, clinical
observations and monitoring activities will be used to evaluate
nurses' compliance with the guideline and skill competencies
related to stoma care. Patient outcomes, as assessed by indicators
such as stoma complications, infection and readmission rates,
will also be monitored, even though it is acknowledged that
direct cause-effect inferences cannot be confirmed between
nurses' compliance with the guideline and these outcome indicators.
Process variables associated with the evaluation of the education
phase of the guideline implementation may include: (1) number
of staff who attended the training sessions; (2) number of
units involved in the training; (3) hours spent in training
sessions; and (4) resources used in the training process.
Outcome variables that will be assessed related to the education
include: (1) staff knowledge and skill related to the guideline
content; (2) guideline utilization and provider compliance
with the standard of care, (3) staff satisfaction with the
teaching/learning process, (4) staff satisfaction with access
to resources during regular hours and after hours.
Other potential evaluation methods could include chart audits,
informal interviews with staff and patients, as well as anecdotal
comments collected in unit log books. These data will provide
baseline information that can be used for comparison over
time. A mechanism will be established to ensure the tracking,
reporting and resolution of problems encountered by staff
and to record gaps in guideline content.
4.1.4 Sustainability
Sustainability of the ostomy practice guideline is at risk
if knowledge contained within it becomes outdated or irrelevant
to current practice and if point-of-care practitioners do
not see the value of integrating best practice principles
into their daily care giving activities. Sustainable change
will be easier to maintain if guidelines are embedded into
electronic documentation and decision supports within the
organization [24]. The project lead (entry level ACNS) will
explore how the ostomy guideline can be linked with the clinical
information system currently being implemented in the corporation.
4.2 Ostomy Guideline Implementation in the GCC Cultural
Context
As noted previously, rates of colorectal cancer are increasing
in Qatar [25, 26] and clinician interest in standardizing
treatment practices has become a national priority [2, 9,
27]. Besides considering the health system context, guideline
implementation must consider the demographic, cultural and
religious context into which the guideline is introduced.
4.2.1 Cultural Challenges and Opportunities
The total population in Qatar is just under 2.5 million [28].
About 80% live in the capital city of Doha and another 10%
live in other urban areas of the country [29]. Population
demographics reflect a diverse cultural mix. Arab nationals
(approximately 0.3 million) comprise less than 15% of the
population. The vast majority of the population consists of
expatriates from multiple countries. Indians and Nepalese
represent the largest groups (1 million combined) and Filipinos
and Egyptians (0.4 million combined) are the other most prevalent
cultural groups.
Over 75% of people living in Qatar practice the Islamic faith;
there is a mix of Arab and non-Arab Muslims. Christians (8.5
- 10%) and other religions, such as Hinduism and Buddhism
make up the remaining population. Similar to neighboring GCC
countries, Qatar has a high proportion of young male construction
workers from low income countries in the Eastern Mediterranean,
South-East Asia, Western Pacific and African regions. As a
result, there is a disproportionate male:female ratio (75:25)
[28].
As Islam is the dominant religion in this culturally diverse
country, a challenge for health professionals is to understand
how culture and religion influence health, self-concept and
response to illness. Authors note that spiritual affiliation
and strength of faith are basic elements of one's cultural
identity [30]. Though there is abundant research describing
the cultural and religious aspects of caring for Muslim patients
[31, 32, 33, 34, 35], there is scarce evidence describing
Muslim patients' stressors and responses to stoma surgery.
In multicultural, Muslim societies such as Qatar, the provision
of culturally competent care requires that health professionals
provide individualized, holistic care that attends to the
spiritual, cultural, psychosocial, interpersonal and clinical
needs of all persons [35]. Cultural competence involves integrating
cognitive and affective components essential for establishing
culturally-relevant relationships between patients and providers
[36].
The preliminary gap analysis completed for this local guideline
adaptation project, revealed that health care providers, including
staff nurses and physicians, do not consistently perform comprehensive
patient/family assessments on persons with ostomy. The focus
of assessment tends to be on physical aspects of care (e.g.
stoma site, signs and symptoms). Less attention is directed
to psychosocial, sexual, cultural, spiritual, and religious
assessment. Dieticians, pharmacists, physiotherapists and
social workers are not regularly involved in patient consultation.
Project team members recognized that these disciplines should
become part of the colorectal team.
Gap analysis also revealed that all patients may not receive
similar information in the pre-operative phase of care. For
instance, those who do not speak one of the dominant languages
(Arabic or English) may miss formal pre-op education. Self-care
practices related to ostomy management may vary within and
between cultural groups or religions. Evaluation measures
have not been formalized to assess patient/family understanding
of self care practices that ensure safe, proficient use of
ostomy products and appliances. These issues represent targets
for improvement.
Beyond cultural and spiritual factors, other demographic variables
challenge the provision of culturally competent care. For
instance, language, income and education level are crucial
issues to assess in Qatar since a large proportion of the
population are migrant workers who do not speak Arabic or
English. This may impede the ability of professionals to communicate
and deliver consistent information to all patients. Culturally
appropriate services (education, counselling, resources, supports)
that consider language and literacy levels must be thoughtfully
planned and customized for patients and families. Studies
of expatriate workers in Kuwait with cancer revealed that
language negatively impacted the adequacy of oncology care
for both Arab-speaking and non-Arab speaking patients. This
relates to the fact that, similar to Qatar and other GCC countries,
many expatriate health care professionals do not speak Arabic
or other languages of patients [37, 38].
Literature indicates the main challenges specific to ostomy
care and religious beliefs of Muslims evolve around hygiene
and prayer, gender and modesty, as well as sexuality and body
image. Following stoma surgery, the individual's body image
and/or self esteem may be altered; perceptions of attractiveness
may have changed and feelings about sexuality may be negatively
impacted [16,39]. These issues may be particularly relevant
for women, owing to the ideals that society places on them
to reflect a positive sexuality and attractive body image
[40]. A Jordan study of Muslim women experiencing bodily changes
during critical illness distinguished three areas of patient
concern: the physical body, the social body and the cultural
body [41]. Jordanian women's dependence on health professionals
for physical care was perceived as reduced performance and
bodily strength which triggered feelings of shame, burden
and helplessness. An altered physical condition was seen by
the women as an inability to contribute normally to family
role functions which induced feelings of social inadequacy.
Female Muslim participants also viewed physical illness as
a threat to their cultural identity due to Islamic beliefs,
customs and expectations regarding women's role in the family
and community.
Having an ostomy forces an individual of the Islamic faith
to confront and adapt to issues pertaining to religious customs.
For Muslims, stoma formation may interfere with their daily
prayer rituals. They must ensure the cleanliness of their
clothes, physical body and place of prayer (5 times / day);
the practice of washing [ablution] prior to prayer, after
sexual intercourse, urination and defecation is rooted in
Islamic ideology [42]. Muslim patients with ostomy may experience
spiritual conflict, not only by the sight of bodily fluids,
but by the perception that they are "unclean".
Research has documented that Muslim patients with stoma report
a more negative quality of life than non-Muslim patients.
This has been attributed to their cessation of daily washing
rituals, mosque visits and prayers. Study participants conveyed
that physiologic factors, such as uncontrolled flatus and
visible faeces, resulted in their inability and/or unwillingness
to observe normal religious customs specific to prayer. As
a result, they experienced social isolation and decreased
quality of life [42]. This reinforces that Muslem patients
with ostomy face unique cultural and religious challenges
that may induce intense conflict and stress. Guideline content
must include comprehensive assessment, as well as resources
and services to address the unique psychosocial and spiritual
support needs of patients.
Privacy, modesty and dignity issues, important to all people
regardless of culture or religion, may have special significance
to Muslim patients with ostomy. Muslim custom related to modesty
requires that clothing cover the entire body, neck and head
and must not be tight, sheer or unduly conspicuous. Muslim
apparel and adherence to modest dress standards may be a source
of comfort to a person with ostomy, serving to limit public
scrutiny or perceived exposure of his/her altered physical
body. Islamic modesty rules also place restrictions on privacy,
the mention of bodily functions and gender relationships [43].
For example, direct eye contact with the opposite sex outside
the family is forbidden for some Muslims and same-sex medical
care providers are generally preferred.
Islamic tradition posits that one's privacy is integral to
his/her dignity [44]. Evidence indicates that "Muslim
women specifically and Arab women in general do not tolerate
unnecessary exposure of their bodies" [45]. Externalizing
the bowel may have a devastating impact on a Muslim woman's
self-image and personal sense of dignity. Because it is not
customary for people of the Muslim faith to discuss sensitive
issues related to bodily functions [43, 46], psychological,
social, and religious supports should be available to assist
individuals to disclose feelings about altered body image
following stoma surgery [39]. On the other hand, research
has shown that strong religious affiliation can have a positive
effect on body image, possibly by redirecting judgments about
self-worth away from appearance and towards moral and ritualistic
pursuits relevant to an individuals' faith [47]. The 21 countries
in the Eastern Mediterranean Health Region [48] are Muslim-dominant
societies. However, varied geo-political, economic and social
factors, coupled with demographic diversity, make it impossible
to predict with certainty whether an ostomy guideline adapted
in Qatar will be relevant to the entire Middle East region.
To assess the relevance of the Qatar ostomy guideline to other
areas of the Middle East, clinical stakeholders in those countries
should engage in a collaborative interdisciplinary appraisal
process similar to that described in this paper. Because Qatar
is the first GCC state to take lead in developing and implementing
guidelines for ostomy care, this small Arabian Gulf country
may become a centre of excellence for best practice in this
field, possibly attracting the attention of neighboring countries.
We envision that the introduction of an ostomy care and management
guideline in Qatar for use by nursing and allied health professionals
will be complementary to the medical guideline for colorectal
cancer available through the National Institute for Health
and Care Excellence (NICE) that serves as a practice standard
for GCC and Middle East colorectal surgeons [49]. Integration
of both guidelines is expected to be the beginning of a new
era of best practice for colorectal cancer and ostomy care
consistent with the national vision to create a world class
health system [27].
5. Conclusion:
Experts all agree that clinical practice guidelines developed
in one part of the world may be difficult to implement in
another geographic region. This paper has summarized the systematic
steps involved in appraising the quality, content and relevance
of two different ostomy guidelines developed in North America
to the Middle East context. The goal was to produce a guideline
for use by health care professionals employed in one major
health corporation in the GCC state of Qatar. The process
involved systematic procedures, standardized critiquing instruments
and input from interprofessional team members. The initiative
enabled a graduate nursing student to assert her leadership
by actively liaising with international experts in EBP, BPGs
and ostomy care. It also provided an opportunity for her to
engage locally with interprofessional colleagues and to involve
them in decision-making to define and shape best practice.
The ultimate goal was to ensure a practice guideline exists
to foster the delivery of quality care to patients with ostomy.
The resultant guideline adaptation is expected to support
optimal health outcomes, healthy adjustment, effective self-care
abilities, bio-psycho-social-spiritual well-being and a positive
quality of life, thereby helping patients face the challenges
of living with ostomy with confidence and independence. The
adapted ostomy care and management guideline is intended for
use by staff involved in care of patients in the preoperative,
postoperative and rehabilitation period. Completing implementation
and evaluation of this guideline in the local context is the
next immediate step. A future priority will be to assess the
need for patient-specific ostomy guidelines.
Acknowledgement
S. Abdul Qader is a new MN graduate working as a clinical
nurse specialist in the colorectal program at Hamad Medical
Corporation in Doha, Qatar.
M.L. King is assistant professor in the faculty of nursing
at University of Calgary in Qatar.
References
[1] Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S,
Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer Incidence
and Mortality Worldwide: sources, methods and major patterns
in GLOBECAN 2012. International Journal of Cancer 2014 October;
136(5): E359-386.
[2] Icli F, Akbulut H, Bazarbashi S. Kuzu MA, Mallath, MK,
Rasul KI, Strong S. Syed AA, Zorlu F. Engstrom PF. Modification
and implementation of NCCN guidelines on colon cancer in the
Middle East and North Africa region. Journal of The National
Comprehensive Cancer Network. 2010 July; (8):S22 - S25.
[3] Rasul K, Awidi A, Mubarak A, Al Homsi, U. Study of colorectal
cancer in Qatar, Saudi Medical Journal. 2001 August; (22):705-707.
[4] Wu H, Chau J, Twinn S. Self-efficacy and quality of life
among stoma patients in Hong Kong. Cancer Nursing. 2007 May;
30(3):186-193.
[5] Burch J. Stoma care in the community. British Journal
Of Community Nursing. 2014 August; 19(8):396-400.
[6] Field M, Lohr K. Guidelines for clinical practice: From
development to use. National Academy Press.Washington:DC;
1992.
[7] Harrison M, van den Hoek J. Canadian Guideline Adaptation
Study Group. CAN-IMPLEMENT: A guideline adaptation and implementation
planning resource. Queen's University School of Nursing and
Canadian Partnership against Cancer, Kingston, Ontario, Canada;
2012.
[8] Locatelli F, Andrulli S, Del Vecchio L. Difficulties of
implementing clinical guidelines in medical practice. Nephrol.
Dial. Transplant. 2000 September; (15), pp. 1284-1287.
[9] Jazieh A, Azim H, McClure J, Jahanzeb, M. The Abu Dhabi
Declaration: The process of NCCN guidelines adaptation in
the Middle East and North Africa region. Journal of the National
Comprehensive Cancer Network. 2010 March; 8 (S3): S2-4
[10] Harrison M, Légaré F, Graham I, Fervers
B. Adapting clinical practice guidelines to local context
and assessing barriers to their use. CMAJ: Canadian Medical
Association Journal. 2010 February; 182(2):E78-84.
[11] Sackett D, Rosenberg W, Gray J, Haynes R, Richardson
W. Evidence based medicine: what it is and what it isn't.
Clinical Orthopaedics & Related Research. 2007 February;
455:3-5.
[12] Cullum N, Ciliska D, Haynes B, Marks S. Evidence-based
Nursing: An Introduction. Oxford, UK: Blackwell Publishing;
2008.
[13] Wells N, Free M, Adams R. Nursing research internship:
enhancing evidence-based practice among staff nurses. Journal
of Nursing Administration. 2007 March; 37(3):135-143.
[14] Novak D, Dooley S, Clark R. Best practices: understanding
nurses' perspectives. Journal of Nursing Administration. 2008
October; 38(10):448-453.
[15] Winch S, Creedy D, Chaboyer W. Governing nursing conduct:
the rise of evidence-based practice. Nursing Inquiry. 2002
September; 9(3):156-161.
[16] Registered Nurses' Association of Ontario (RNAO), Ostomy
Care and Management, RNAO: Toronto, ON; 2009.
[17] Wound, Ostomy, and Continence Nurses Society (WOCNS).
Management of the patient with a fecal ostomy: best practice
guideline for clinicians, WOCNS: Mount Laurel, New Jersey;
2010.
[18] The AGREE II Collaboration, Appraisal of guidelines for
research and evaluation: AGREE II instrument. 2009. http://www.agreetrust.org.
[19] Burgers J, Fervers B, Cluzeau F, et al. International
assessment of the quality of clinical practice guidelines
in oncology using the Appraisal of Guidelines and Research
and Evaluation Instrument. Journal of Clinical Oncology. 2004
May; 22(10):2000-2007.
[20] Graham I, Harrison M. EBN users' guide. Evaluation and
adaptation of clinical practice guidelines. Evidence Based
Nursing. 2005 July; 8(3):68-72.
[21] Melnyk B, Fineout-Overholt E. 2nd ed. Evidence based
practice in nursing & health care. A guide to best practice.
Wolters Kluwer Lippincott Williams & Wilkins: Philadelphia,
PA; 2011.
[22] Groot P, Hommersom A, Lucas P. Adaptation of clinical
practice guidelines. Studies in Health Technology & Informatics.
2008 September; 139:121-139.
[23] Kalisch B, Boqin X, Ronis D. Train-the-trainer intervention
to increase nursing teamwork and decrease missed nursing care
in acute care patient units. Nursing Research. 2013 December;
62(6), 405-413. doi:10.1097/NNR.0b013e3182a7a15d
[24] Dowding D. Computerized decision support systems in nursing.
Cullum N et al. Evidence-based nursing: An Introduction. Oxford:
Blackwell Publishing; 2008.
[25] Bar-Chana M, Ibrahim AS, Mikhail N. MOS Epidemiology
Group Special Report: cancer incidence in Mediterranean populations.
Mediterranean Oncology Society, 2009 http://www.mosoncology.org/index.php/literature
[26] Bener A, Ayub H, Kakil R, Ibrahim W. Patterns of cancer
incidence among the population of Qatar: a worldwide comparative
study. Asian Pacific Journal of Cancer Prevention 2007 8(9),19-24.
[27] Brown R, Kerr, K. Haoudi, A. Darzi, A. Tackling cancer
burden in the Middle East: Qatar as an example. The Lancet
2012 November, 13: 2501-e508. www.thelancet.com/oncology
[28] Qatar's Ministry of Development Planning and Statistics.
[Internet]. Qatar, 2014.[ updated December July 2014]. Available
from: http://www.bqdoha.com/2013/12/population-qatar
[29] Agy SN. Countries and their cultures [Internet]. Qatar,
2015. Available from: http://www.everyculture.com/No-Sa/Qatar.html.
[30] Tarakeshwar N, Stanton J, Pargament K. Religion: An overlooked
dimension in cross-cultural psychology. Journal of Cross-cultural
Psychology.2003 July ;34, 377-394.
[31] Marrone S. Factors that influence critical care nurses'
intentions to provide culturally congruent care to Arab Muslims.
Journal of Transcultural Nursing. 2008 January ;19(1), 8-15.
[32] Simpson J, Carter K. Muslim women's experiences with
health care providers in a rural area of the United States.
Journal of Transcultural Nursing. 2008 January ;19(1), 16-23.
[33]Al-Shahri M.Z. Culturally Sensitive Caring for Saudi Patients.
Journal of Transcultural Nursing. 2002 April ;13 (2), 133-138.
[34]Yousef A. Health beliefs, practice, and priorities for
health care of Arab Muslims in the United States: Implications
for nursing care. Journal of Transcultural Nursing. 2008 July;19(3),
284-291.
[35] Lovering S. (2012). The Crescent of Care: a nursing model
to guide the care of Arab Muslim patients. Diversity and Equality
in Health and Care. 2012 September; 9,171-178
[36] Alexander GR. Cultural competence models in nursing,
Nursing Clinics of North America. 2008 December; 20(4): 415-421.
[37] Alshemmari SH, Refaat S, Elbashmi AA, AlSirafy S. Representation
of Expatriates Among Cancer Patients in Kuwait and the Need
for Culturally-Competent Care. Journal of Psychosocial Oncology
2012 30: 380-385.
[38] Ayanian JZ, Zaslavsky AM, Guadagnoli E, Fuchs CS, Yost
KJ, Creech, CM, . . . Wright, WE. Patients' perceptions of
quality of care for colorectal cancer by race, ethnicity,
and language. Journal of Clinical Oncology, 2005 23: 6576-6586.
[39] Kuzu MA , Topçu O, Uçar K, Ulukent S, Unal
E, Erverdi N, Elhan A, Demirci S. Effect of sphincter-sacrificing
surgery for rectal carcinoma on quality of life in Muslim
patients. Dis Colon Rectum. 2002 October;45(10):1359-66
[40] Grogan S. Body Image: Understanding Body Dissatisfaction
in Men, Women and Children. 2nd ed. Routledge, New York; 2008.
[41] Zeilani R, Seymour JE. Muslim Women's Narratives About
Bodily Change and Care During Critical Illness: A Qualitative
Study. Journal of Nursing Scholarship. 2012 December ; 44
(1), 99-107.
[42] Black P. Understanding religious beliefs of patients
needing a stoma. Gastrointestinal Nursing. 2011December; 9(10):17-22.
[43] Rashidi A, Rajaram SS. Middle Eastern Asian Islamic women
and breast self-examination: needs assessment. Cancer Nursing.
2000 February;23, 64-70.
[44] Kamali MH. The Dignity of Man: An Islamic Perspective.
Cambridge, England: The Islamic Texts Society.2002.
[45] Hammoud MM, White, CB, Fetters MD. Opening cultural doors:
Providing culturally sensitive healthcare to Arab American
and American Muslim patients. American Journal of Obstetrics
and Gynecology. 2005 October ;193, 1307-11.
[46] Andrews CS. Modesty and healthcare for women: understanding
cultural sensitivities. Community Oncology.2006 July; 3 (7):
443-446.
[47] Ferraro KF. Firm believers? Religion, body weight, and
well-being. Review of Religious Research. 1998 March ;39,
224-244.
[48] World Health Organization. Countries [Internet]. 2011.
Available from: http://who.net/countries/en/.
[49] National Institute for Health and Quality Excellence
(NHS). The diagnosis and management of colorectal cancer -
NICE quality standard 131. 2014 December: 1-50. Available
from: https://www.nice.org.uk/guidance/cg131.
|
 |