| |
April
2015
- Volume 9, Issue 2
Evidence Based Practice: Aerobic Exercise and Major Depressive
Disorder

|
 ( (
|
Yousef Qan`ir
Correspondence:
Yousef A. Qan'ir,
M.Sc., RN
Master Degree in Nursing
The Hashemite University
Zarqa, Jordan
P.O. Box 150459, Zarqa 13115,
Jordan
Email: Yousefqaneer@hotmail.com
|
 |
|
Abstract
Major Depressive Disorder (MDD) is one of the common
health problems, and is estimated to affect 121 million
adults worldwide. MDD is a recurrent illness, with high
incidence of returning, and the risk of relapse that
increases as the number of previous episodes increase.
Hence, the choice of treatment is important to improve
the quality of life and to prevent or minimize recurrent
episodes. Physical exercise is an example of alternative
and complementary therapy that has received considerable
and significant attention in the treatment of MDD. The
efficacy of aerobic exercise approaches is considered
and has a place in mental health practice. According
to many studies aerobic exercise is the preferred form
of exercise for patients with MDD. Moreover, Aerobic
exercise has been proven as an effective treatment for
MDD, and there are sufficient studies to help health
care providers to prescribe aerobic exercise as a treatment
choice for MDD patients. It is recommended that patients
participate in three to five exercise sessions per week,
for 30 to 45 minutes per session. Within the range of
intensity for aerobic exercise, that achieves a level
of heart rate of 70 to 85 % of the heart rate reserve.
Furthermore, the majority of research emphasizes that
the exercise regimen should be continued for at least
10 to 16 weeks to achieve the greatest antidepressant
effect.
Key words: Aerobic Exercise; Major Depression.
|
Introduction
Mental health problems are international challenges that have
a significant contribution in illness burden over the entire
world (Blake, 2012). Major Depressive Disorder (MDD) is one
of the common health problems, and is estimated to affect
121 million adults worldwide (World Health Organization [WHO],
2012). Projections for the year 2030 indicate that MDD will
rank second only to coronary heart disease as a cause of illness
burden over the entire world (WHO, 2012). Furthermore, WHO,
2012 reported that MDD currently represents a second health
problem regarding disability caused by illness in the world.
MDD is associated with significant morbidity, mortality, and
disability that burden the individual and his family, and
contribute to impaired cognitive skills and deterioration
of the individual life aspects (Blake, 2012; Nahas & Sheikh,
2011). Many risk factors are associated with incidence of
MDD as genetic factors, life events, sleeping disturbance,
alcohol, and some drugs (Townsend, 2011). Symptoms of depression
include feeling of hopelessness and helplessness, loss energy,
anhedonia, agitation, fatigue, withdrawn, weight loss or gain,
fatigue and inappropriate thinking (Townsend, 2011).
MDD is a recurrent illness, with high incidence of returning,
and the risk of relapse increases as the number of previous
episodes increase (Solomon, Keller, Leon, Mueller, & Lvori,
2000). Hence the choice of treatment is important to improve
the quality of life and to prevent or minimize recurrent episodes.
For instance, the majority of western guidelines published
since 2000 have similar recommendations about all stages of
treatment of depression, that is first line treatment is usually
serotonin reuptake inhibitor, psychotherapy, or combination
of psychotherapy and pharmacotherapy (Gelenberg, 2010). Indeed,
no single treatment for MDD is effective for every patient
(Nahas & Sheikh, 2011). Almost half of depressed patients
who are treated do not attain full remission of their symptoms
of MDD and they remain under risk of residual symptoms and
relapse (Solomon et al., 2000). Allopathic therapies could
be undesirable options for MDD management illustrated by antidepressant
medications having unpleasant side effect, and psychotherapy
could be time consuming and expensive (Demyttenaere et al.,
2001). Many depressed patients choose complementary alternative
medicine instead of allopathic (Solomon et al., 2000). Hence,
there is a great interest in development of alternative and
complementary therapies to enhance and promote treatment options
of MDD (Blake, 2012).
Physical exercise is an example of alternative and complementary
therapy that has received considerable and significant attention
in treatment of MDD (Blake, 2012). Physical exercise may be
a viable treatment because it can be recommended for any patient
at any time without suffering a negative social stigma (Nahas
& Sheikh, 2011). In general, physical exercise has a significant
and clear positive effect on physical health and psychological
process in the human body (Blake, 2012). Normal physical health
conditions may play a significant role in mental health balance,
and maintain biopsychological aspect in the human body (Helmich
et al., 2010). A number of studies indicated a consistent
association between improving mental health and regular physical
exercise (Hassmen, Koivula, & Uutela, 2000). In addition,
many studies reported that physical exercise might reduce
depressive symptoms in the nonclinical population and in patients
diagnosed with MDD (Nahas & Sheikh, 2011). At the same
time, an association between physical inactivity and higher
levels of depressive symptoms in patients with MDD is observed
(Helmich et al., 2010).
Concept of physical exercise indicates regular, structured,
continuous, rhythmical fashion, and leisure time activity
(Hassmen et al., 2010). Specifically, aerobic exercise is
a kind of exercise which involves prolonged activity of large
muscle groups to produce energy by metabolizing oxygen; such
as running, swimming, and aerobic dancing (Reed & Buck,
2009). Unlike aerobic exercise, anaerobic exercise reflects
intense, brief, and nonsustainable muscular activities that
use the energy to produce activity without inhaling oxygen;
such as in weight lifting, and pushing down (Reed & Buck,
2009).
In fact, the majority of healthy people prefer and use this
kind of exercise in their life activities, and aerobic exercise
is one of the common exercise modalities that is recommended
for mental health improvement (Reed & Buck, 2009). Many
studies have examined its effectiveness and viability to manage
mental disorders (Kanning & Schlicht, 2010). Moreover,
the efficacy of aerobic exercise approaches is considered
and has a place in mental health practice, but some researchers
suggested inconsistent recommendations regarding adoption
of aerobic exercise as treatment choice for MDD (Reed &
Buck, 2009).
Dose, Frequency, and Technique of Aerobic
Exercise for MDD Management
The efficacy of aerobic exercise in treatment of MDD may be
affected by age and severity of symptoms, but intensity of
exercise programs have a substantial impact on aerobic exercise
effectiveness for MDD (Silveira et al., 2013). Determining
the type of exercise for people with MDD has to focus on personal
interest, physical needs, risk for injury, and adverse effects
for current medication. Selecting the convenient exercise
is primary for continued consistent exercise intensity (Silveira
et al., 2013).
In a report of 2013, American College of Sports Medicine (ACSM)
defined many concepts related to intensity of aerobic exercise.
In the beginning, ACSM used heart rate reserve term to reflect
exercise intensity that is equivalent to the desired percentage
of maximal oxygen uptake. Heart rate reserve means the difference
between resting heart rate and maximum heart rate. ACSM set
maximum heart rate as the highest number of beats per minute
during physical exertion, and resting heart rate is the lowest
number of heart beats per minute during ful relaxation and
without distractions. The intended increase in heart rate
reserve means increase in the aerobic exercise intensity (ACSM,
2013). Additionally, ACSM articulated that exercise intensity
reflects how much energy is expended when exercising. ACSM
clarifies a way to optimize energy expenditure by modifying
the intensity of the exercise. It is important to choose mode
of exercise that can be regulated to overload the cardio respiratory
system and increase the heart rate reserve level, so it will
increase exercise intensity (ACSM, 2013).
ACSM (2013) classified exercise mode for MDD treatment regarding
energy expenditure into three groups of exercise (a) exercises
that provide a consistent intensity and energy expenditure
such as walking, jogging, cycling, and stair climbing; (b)
in this group the exercise will burn more calories if a person
worked harder and longer such as aerobic dancing, bench stepping,
and swimming; (c) large muscle contractions with prolonged
activities such as basketball, racquet sports, and volleyball
are high energy expenditure exercise activities. Moreover,
many doses are used to determine energy expenditure in an
aerobic exercise program,for instance, public health dose
of aerobic exercise that is total weekly energy expenditure
of 17.5 kcal/kg/wee k, and low dose aerobic exercise that
is total weekly expenditure of 7 kcal/kg/week (ACSM, 2013).
More energy expenditure means more effective exercise practice
because of the biophysiological actions of muscle contractions,
and hormonal excretion after intensive exercising program
(Drevets, 2001).
Aerobic exercise program for MDD. In their study, Dunn et
al. (2005) reported that aerobic exercise consistent with
public health dose is an effective treatment for MDD, but
a lower dose is comparable to no treatment intervention. Dunn
et al. also concluded that there was no difference in result
between 3 days per week of aerobic exercise and 5 days per
week. Hence, the distinct factor for reduction of MDD symptoms
is total energy expenditure not frequency of exercise sessions.
In the same way, Blumenthal, Smith, and Hoffman (2012) concluded
that no differences between 3 days per week and 5 days per
week of aerobic exercise as a therapeutic exercise regimen
for MDD, but exercise adherence is the essential factor to
profit from the exercise program.
Blumenthal et al. (1999) applied 16 weeks exercise program
of 45 minutes session per day for three days every week on
MDD participants. The result showed positive outcomes after
implementing this method, and the exercise program achieved
therapeutic effects (Blumenthal et al., 1999). Another design,
which is developed by Davidson (2010) within a guideline for
MDD treatment, presented a different aerobic exercise program.
Davidson's program consisted of three times weekly of regular
walking and jogging sessions for 10 weeks; each exercise session
consisted of 10 minutes of stretching exercise, followed by
45 minutes of continuous walking or jogging to obtain desired
exercise intensity by increasing heart to 70-85% of maximum
heart rate of MDD participant. A somewhat distinct aerobic
exercise program performed by Babyak et al. (2000) and Blumenthal
et al. (2007) suggested three exercise sessions per week for
16 consecutive weeks. Every session designate training exercise
ranges equivalent to 70-85 % of heart rate reserve. Each aerobic
session started with 10 minutes warm up period, next followed
by 30 minutes of brisk walking or jogging at intensity consistent
with assigned heart rate reserve. After that, exercise session
concluded with five minutes of cool down exercise. The exercise
program achieved positive results in managing symptoms of
MDD (Babyak et al., 2000; Blumenthal et al., 2007). A positive
outcomes study by Hoffman et al., (2011) applied similar aerobic
exercise method within their randomized clinical trial study
to reduce MDD symptoms. Hoffman et al. designed program of
attending 45 minutes of aerobic exercise of running, jogging,
and treadmill each week for four months within target heart
rate of 70-85% of heart rate reserve.
Briefly, three days of aerobic exercise sessions per week
for consecutive weeks range from 10 to 16 weeks; every session
of jogging, running, walking, or treadmill, or any aerobic
exercise that the patient is interested in, continued for
30 to 45 minutes, and maintained at 70 to 85 % of monitored
heart rate reserve. Also consideration should be given to
the patients` abilities for these exercise sessions in regard
to their health, time, and willingness for exercise practice,
could be an appropriate program for MDD management practice.
PICO Format
Evidence-based practice is integration
of best research evidence with clinical expertise and patient
values (Stuart, 2001). To implement evidence based practice
strategies, we can use PICO, which is a method of putting
together a search strategy that allows the health care provider
to take a more evidence-based approach to the literature searching
when searching bibliographic databases (Stuart, 2001).
A clinical question needs to be directly relevant to the patient
or problem. It needs to be phrased in such a way as to facilitate
the search for an answer. PICO makes this process easier (Stuart,
2001). It is a memorial for the important parts of a well-built
clinical question. It also helps formulating the search strategy
by identifying the key concepts that need to be in the article
that addresses the question. A PICO question consists of four
elements (a) population or patients (b) intervention (c) comparison
(d) outcome.
At this level, we can clarify current clinical questions that
articulate the efficacy of aerobic exercise to manage patients
with MDD. Furthermore, it could compare aerobic exercise to
antidepressant in managing MDD. PICO questions apply a convenient
format that will ease process of answering relevant questions.
PICO search strategies will consider the main elements of
PICO questions. Proposed PICO questions elements are illustrated
in Table 1.
Table 1

PICO Questions
Clinical elements are combined through PICO format to formulize
PICO questions. The proposed three PICO questions are:
1- In patients with MDD, does aerobic exercise program
reduce the symptoms of MDD?
2- In patients with MDD, what is the effect of aerobic
exercise program on reducing symptoms of MDD compared to no
aerobic exercise?
3- In patients with MDD, how does aerobic exercise
program compared with antidepressant reduce
symptoms of MDD?
Literature
Review
Effects of Aerobic Exercise on People with MDD
In this situation, one systematic review performed by Phillips,
Kiernan and King (2003) indicated that aerobic exercise has
beneficial effects on patients with MDD, and may increase
social integration, successful adaptation, and self esteem
of patients with MDD. In addition, Phillips et al. (2003)
reported that an aerobic exercise as little as four weeks
could beneficially affect people with MDD. Similarly, Lawlor
and Hopker (2001) in their systematic review concluded that
aerobic exercise may be efficient in reducing symptoms of
depression among patients with MDD in the short term, but
it is not clear for long term treatment plan due lack of follow
up studies.
A number of randomized clinical trials studies examined the
effects of aerobic exercise on people with MDD. For instance,
Carter, Callaghan, Khalil and Morres (2012) found that sufficient
intensity of aerobic exercise has effective outcome on the
depressive symptoms of patients who are experiencing MDD.
Equally, another randomized clinical trial conducted by Dunn,
Trived, Kampert, Clark, and Chambliss (2005) concluded that
standard aerobic exercise is an effective treatment for MDD
of mild to moderate severity. The authors suggested that participants
with MDD who underwent the study showed an improvement in
their mental status after implementing a full aerobic exercise
program (Dunn et al., 2005). In the same way, in 2007, Blumenthal
et al. in their randomized clinical trial study showed that
aerobic exercise program for participants with MDD is better
than no treatment intervention to improve mood status. In
a like manner, one randomized clinical trial reported that
MDD patients positively interested in aerobic exercise, showed
efficacious response after a modest exercise program (Babyak
et al., 2000). Particularly, aerobic exercise is an effective
and potent treatment for patients with MDD in case the patients
are willing to undergo the exercise program (Babyak et al.,
2000). One quasi-experimental study reported that aerobic
exercise program decreased the depression scores in Hamilton
rating scale among elderly women who experienced MDD (Sayyad,
Nazer, ansary, & Khleghi, 2006). Furthermore, in their
pilot study Dimeo, Bauer, Varahram, Proest, and Halter (2001)
concluded that an improvement in mood status could occur after
implementing 10 days of aerobic exercise for patients experiencing
mild MDD.
In contrast, one randomized clinical trial conducted by Krough,
Videbech, Thomsen, Gluud, and Nordentoft (2012) indicated
opposite outcomes to previous studies. Study of Krough et
al. concluded that aerobic exercise has no significant effect
on patients who experienced MDD. Additionally, Krough et al.
reported that duration, frequency, and intensity of aerobic
exercise are not substantial to potentiate aerobic exercise
performance. Another randomized clinical trial showed that
one year of exercise training is not effective for depressive
symptoms among residents of care homes and nursing homes who
are experiencing MDD (Underwood et al., 2013).
Aerobic Exercise versus Antidepressant
Medication
Aerobic exercise may reduce negative side effects of antidepressants,
such as fatigue, dizziness, and constipation, thus increasing
compliance in medication use (Kruisdijk, Hendriksen, Tak,
Beekman, & Rock, 2012). Aerobic exercise could be applied
as a single treatment plan or complementary therapy in addition
to pharmacological treatment (Kruisdijk et al., 2012). No
doubt, adverse effects of aerobic exercise are less than antidepressant,
and aerobic exercise is relatively safer than antidepressant
with low cost charges (Kruisdijk et al., 2012).
One systematic review showed that aerobic exercise and antidepressant
medication are similar regarding reduction of depressive symptoms
on the Hamilton depression rating scale in patients diagnosed
as MDD (Danielsson, Noras, Waern, & Carlsson, 2013). The
same review recommended that people with MDD should be treated
with aerobic exercise instead of antidepressant medication
(Danielsson et al., 2013). Another meta-analysis concluded
aerobic exercise enhances the response to antidepressant treatment
for MDD patients, but it is less effective than antidepressant
treatment in improving MDD symptoms (Silveira et al., 2013).
On other hand, Cooney et al. (2013) concluded in their systematic
review that aerobic exercise is slightly more effective than
no treatment intervention to reduce depressive symptoms among
MDD patients, but is less effective than pharmacological treatment
in reducing depressive symptoms or improving quality of life
for people with MDD.
Another clinical trial study suggested that the effect of
aerobic exercise on MDD remission is similar to antidepressant,
and aerobic exercise may enhance the efficacy of pharmacological
treatment (Hoffman et al., 2011). This conclusion is supported
by another randomized clinical trial conducted by Blumenthal
et al. (2007) who found efficacy of exercise treatment similar
to antidepressant medications, and both treatments are better
than no treatment intervention in patients with MDD. Also,
an earlier study completed by Blumenthal et al. (1999) suggested
more positive expectation regarding aerobic exercise which
may be considered as alternative treatment to antidepressants
to manage MDD. However, some antidepressants may provide rapid
onset therapeutic response more than aerobic exercise that
enhances position of antidepressant medications as the first
line treatment for MDD (Blumenthal et al., 1999).
Discussion
In general, many studies of first level of evidence concluded
that aerobic exercise is effective in reducing symptoms of
patients with MDD. All studies that reported positive outcomes
regarding aerobic exercise efficacy in MDD are summarized
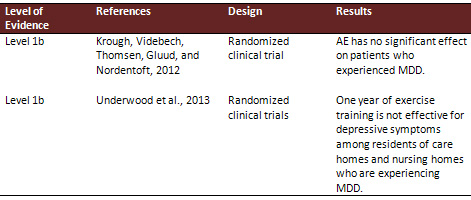
in Table 2. However, as shown in Table 3, two randomized clinical
trial studies showed that aerobic exercise has no effect in
reducing symptoms of MDD. Hence, the clinical questions, which
investigate the efficacy of aerobic exercise and compare it
to no treatment approaches, could be answered after evaluating
all relevant studies.
Click here for Table 2: Summary
of Positive Results Studies for efficacy of AE in MDD
The systematic review and randomized clinical trial studies
articulated a positive relation between aerobic exercise and
reducing symptoms of MDD. High level of evidence in these
studies affords capacity to answer the clinical questions.
No doubt, number and level of evidence of former studies,
that found aerobic exercise is effective in reducing symptoms
of MDD, are more vigorous than studies that showed negative
outcomes.
Searching of literature related to PICO questions that compare
aerobic exercise to antidepressant, found high level of evidence
as represented in Table 4. The studies reported that aerobic
exercise may be similar or less efficient than antidepressant
in reducing symptoms of MDD. However, no studies showed opposite
outcomes. Similarly, aerobic exercise could not be more effective
than antidepressant in reducing symptoms of MDD.
Table 3
Click here for Table 4:
Summary
of Studies for Efficacy of AE versus Antidepressant
Summary
According to former studies aerobic exercise is the preferred
form of exercise for patients with MDD. Moreover, Aerobic
exercise has been proven as an effective treatment for MDD,
and there are sufficient studies to help health care providers
to prescribe aerobic exercise as a treatment choice for MDD
patients. The results showed that patients may experience
a relief in depressive symptoms in as little as four weeks
after starting exercise.
Although a question whether patients with MDD could actually
participate in an aerobic exercise program, the studies suggested
that the majority of MDD patients prefer the aerobic exercise
rather than antidepressant medication and MDD patients drop
out rate from the exercise programs is very low.
It is recommended that patients participating in three to
five exercise sessions per week, for 30 to 45 minutes per
session. Within the range of intensity for aerobic exercise,
that achieves a level of heart rate of 70 to 85 % of the heart
rate reserve. Furthermore, the majority of research emphasizes
that the exercise regimen should be continued for at least
10 to 16 weeks to achieve the greatest antidepressant effect.
The recommended strategies that may help improve adherence
to exercise programs, include asking patients about their
favorite type of exercise, and encouraging them by using a
group exercise program. In addition, it is recommended also
to encourage patients to engage in at least some exercise,
even if they do not exercise enough to meet current public
health dose exercise, they may take a first step in this therapeutic
approach.
It is also recommended more research studies should be carried
out in this area with emphasis on methodological accuracy,
adequate sample size, and follow up research design with long
term examination methods.
Conclusion
Aerobic exercise could be part of the treatment plan for patients
with MDD even as single treatment therapy, or combined with
other allopathic treatment approaches. In addition, the aerobic
exercise program could be implemented as planned and structured
practice according to available randomized clinical trials
methods of aerobic exercise intervention, which reported that
aerobic exercise is effective to treat MDD, and potentiate
antidepressant medications.
Acknowledgement:
The author extend his appreciation to the College of Nursing
at The Hashemite University; specifically to Professor Dr.
Majd Mrayyan.
References
American College of Sports Medicine. (2013). ACSM's guidelines
for exercise testing and prescription for mental disorders.
Retrieved from http://www.acsm.org/about-acsm/media-room/news-
releases/2013/03/13/acsm-to-preview-9th-edition-of-exercise-mental-
guidelines.pdf.
Babyak, M., Blumenthal, J., Herman, S., Khatri, P., Doraiswamy,
P., Moore, K., Craighead, E. (2000). Exercise treatment for
major depression: maintenance of therapeutic benefit at 10
months. Psychosomatic Medicine, 62(3), 633-638.
Blake, H. (2012). Physical activity and exercise in the treatment
of depression. FrontierPsychiatrist, 106(3), 343-352.
Blumenthal, J., Babyak, M., Doraiswamy, M., Watkins, L., Hoffman,
B., Barbour, K.,… Herman, S. (2007). Exercise and pharmacotherapy
in the treatment of major depressive disorder. Psychosomatic
Medicine; 69(7), 587-596, doi:10.1097/PSY.0b013e318148c19a.
Blumenthal, J., Babyak, M., Moore, K., Craighead, E., Herman,
S., Khatri, P., Waugh, R. (1999). Effects of exercise training
on older patients with major depression. Archive of Internal
Medicine, 159, 2349-2356.
Blumenthal, J., Smith, P., & Hoffman, B. (2012). Is exercise
a viable treatment for depression. ACSMs Health Fitness Journal,
16(4), 14-21.
Carter, T., Callaghan, P., Khalil, E., & Morres, I. (2012).
The effectiveness of a preferred intensity exercise programme
on the mental health outcomes of young people with depression.
BMC Public Health, 12,187.
Cooney, G., Dwan K, Greig C., Lawlor D., Rimer J., Waugh F.,
McMurdo M., & Mead G. (2013). Exercise for depression.
Cochrane Database of Systematic Reviews, 9(1). DOI: 10.1002/14651858.CD004366.pub6.
Danielsson, L., Noras, A., Waern, M, & Carlsson, J. (2013).
Exercise in the treatment of major depression: A systematic
review grading the quality of evidence. Physiotherapy Theory
Practice, 29(8), 573-85. doi: 10.3109/09593985.2013.774452.
Davidson, J. (2010). Major depressive disorder treatment guidelines
in America and Europe. Journal of Clinical Psychiatry, 71(1).
Demyttenaere, K., Enzlin, P., Dewe,W., Boulanger, B., De BieJ,
A., Déja A., Troyer,W., et al. (2001). Compliance with
antidepressants in a primary care setting. Journal of Clinical
Psychiatry, 62(22), 30-33.
Dimeo, F., Bauer, M., Varahram, I., Proest, G., & Halter,
U. (2001). Benefits from aerobic exercise in patients with
major depression: a pilot study. BMJ Sports Medicine, 35,114-117.
Dunn, A., Trivedi, M., Kampert, J., Clark, C., & Chambliss,
H., (2005). Exercise treatment for depression efficacy and
dose response. American Journal of Preventive Medicine, 28(1),1-8.
Gelenberg, A. ( 2010). A review of the current guidelines
for depression treatment. Journal of Clinical Psychiatry,
71(7). doi: 12.419/0878785.2013.7752.
Hassmen, P., Koivula, N., & Uutela, A. (2000). Physical
exercise and psychological well-being: a population study
in Finland. Preventive Medicine, 30, 17-25.
Helmich, I., Latini, A., Sigwalt, A., Carta, M., Machado,
S., Velasques, B., Ribeiro, P., & Budde, H. (2010). Neurobiological
alterations induced by exercise and their impact on depressive
disorders. Clinical Practice & Epidemiology in Mental
Health, 6(1), 115-125.
Hoffman, B., Babyak, M., Craighead, E., Sherwood, A., Doraiswamy,
M., Coons, M., & Blumenthal, J. (2011). Exercise and pharmacotherapy
in patients with major depression: one-year follow-up of the
smile study. Psychosomatic Medicine, 73(2), 127-133. doi:10.1097/PSY.0b013e31820433a5.
Kanning, M., & Schlicht, W. (2010). Be active and become
happy: an ecological momentary assessment of physical activity
and mood. Journal of Sport & Exercise Psychology, 32(2),
253-261.
Krogh, J., Videbech, P., Thomsen, C., Gluud, C., & Nordentoft,
M. (2012). Aerobic exercise versus stretching exercise in
patients with major depression. Public library of science
one, 7(10). doi:10.1371/journal.pone.0048316.
Kruisdijk, F., Hendriksen, I.,Tak, E., Beekman, A., &Rock,
M. (2012). Effect of running therapy on depression. BMC Public
Health; 12:50.
Lawlor, D., Hopker, S. (2001). The effectiveness of exercise
as an intervention in the management of depression. British
Medical Journal, 322, 1-8.
Nahas, R., & Sheikh, O. (2011). Complementary and alternative
medicine for the treatment of major depressive disorder. Canadian
Family Physician, 57(1).
Phillips, W., Kiernan, & M., King, A. (2003). Physical
activity as a nonpharmacological treatment for depression.
Complementary Health Practice Review journal, 8(2), 139-152.
Reed, J., & Buck, S. (2009). The effect of regular aerobic
exercise on positive- activated affect: A meta-analysis. Psychology
of Sport and Exercise, 10(6), 581-94.
Sayyadi, A., Nazer, M., Ansary, A., & Khleghi A. (2006).
The effect of the exercise training on depression in elderly
women. Annals of General Psychiatry, 5(1), 199-203. doi:10.1186/1744-859X-5-S1-S199.
Silveira, H., Moraes, H.,Oliveira, N.,Coutinho, E., Laks,
J., & Deslandes, A. (2013). Physical exercise and clinically
depressed patients: a systematic review. Neuropsychobiology
journal; 67(4), 61-68. DOI:10.1159/000345160.
Solomon, D., Keller, M., Leon, A., Mueller, T., & Lavori,
P. (2000). Multiple recurrences of major depressive disorder.
American Journal of Psychiatry, 157(2), 229-233.
Stuart, G. (2001). Evidence based psychiatric nursing. Journal
of American Psychiatric Nurses association, 7, 103.
Townsend, M. (2011). Essential of Psychiatric Mental Health
Nursing: Concepts of care in evidence-based practice. 5th
Ed. F.A Davis. Philadelphia.p.371.
Underwood, M., Lamb, S., Eldridge, S… et al. (2013).
Exercise for depression in elderly residents of care homes:
a cluster-randomized controlled trial. The Lancet Journal,
382, 41-49.
World Health Organization. (2012). Global burden of disease
report. Disease prevalence and disability. Geneva: WHO; Retrieved
from
www.who.int/mediacentre/events/2012/wha65/journal/en/index4.html
|
 |