| |
April
2015
- Volume 9, Issue 2
Uncontrollable Behavior and Restraints Policy Analysis

|
 ( (
|
Rami Sami
ELshalabi
Correspondence:
Rami Sami ELshalabi,
RN, MSN, CNS
Master Degree Psychiatric and Mental Health Nursing
Clinical Nurse Specialist
Princess Salma
Faculty of Nursing
Al- albayt University,
P.O.BOX 130040, Mafraq, 25113,
Jordan
Email: r.elshalabi@yahoo.com
|
|
Abstract
Aim: To assess and analyze the uncontrollable
behavior and restraint policy for National Center of
Mental Health in Jordan according to administrative
ease, cost and benefits, effectiveness, equity, legality
and political acceptability.
Background: The use of restraint in psychiatric
settings supports to restrict policy and program on
how to deal with uncontrollable behavior as a result
of the decrease in number of restraint patients.
Conclusion: There are many alternatives that
are effective, safe to patient and staff, legal, easy
to apply, and accepted politically, instead of use of
physical restraint.
Key words: Policy, Restrain, Restraint, Patient,
Psychiatric Settings, Uncontrollable Behavior
|
Introduction
Restraint is often used to control the behavior of people
with mental conditions in a variety of settings including
hospitals and psychiatric treatment facilities (Haimowitz,
Urff, Huckshorn, 2006). Psychiatric settings use medical intervention
as a restraint to reduce risk demonstrated by violent patients
from harming themselves and others (Regan, Wilhoite, Faheem,
Wright, & Hamer, 2006). Restraint is an intervention used
in the treatment and management of violent behaviors in psychiatry
(McCue, Urcuyo, Lilu, Tobias, & Chambers, 2004).
The objectives of this policy analysis paper are
A) To assess and analyze the uncontrollable behavior
and restraint policy for National Center of Mental Health
in Jordan, according to administrative ease, cost and benefit,
effectiveness, equity, legality and political acceptability.
B) To suggest an alternative that can be applied in
the National Center of Mental Health.
C) To discuss possible alternatives according to literature.
The MEDLINE, CINAHL and EBSCOhost database were reviewed for
searching the topics; the keywords restrain , restrain policy
were used.
Health policy was defined as "a set course of
action undertaken by governments or health care organizations
to obtain a desired outcome" (Cherry & Jacob, 2007).
Policy analysis is defined as "the systematic study of
background, purpose, content, and anticipated or actual effects
of standing or proposed policies and the study of relevant
social, economic and political factors" (Dye as cited
in Mason, Leavitt, & Chaffee, 2007).
Step One: Verify, define, and
detail the problem
The term restraint includes either physical restraint or chemical
restraint; physical restraint is any manual method or physical
or mechanical device, material, or equipment attached or adjacent
to the patient's body that restricts freedom of movement (Regan,
et al., 2004). Chemical restraint is a medication used to
control behavior or to restrict the patient's freedom of movement
and is not a standard treatment for the patient's medical
or psychiatric condition (Regan, et al., 2006).
Restraints are useful to prevent injury and reduce agitation
but the use of restraint in the treatment of mentally ill
patients is a highly controversial and potentially dangerous
practice (Lewis, Taylor, & Parks, 2009). In addition,
it can produce physical and psychological effects on both
patients and staff (McCue, et al., 2004).
The improper use of restraints can lead to patient harm and
potential civil litigation. The researcher and clinicians
have become focused on physical restraint because of lack
of consensus within the field about the appropriate use of
restraint, damage of therapeutic relationships, in addition
it produces significant physical and psychological risk; including
death related to asphyxia, aspiration, cardiac events brought
on by exertion and medication-interaction (Haimowitz, et al.,
2006). In 2005, a case where a woman was admitted to a county
hospital psychiatric inpatient unit, guards and technicians
restrained her, and during the restraint process, had her
face down on the floor for thirteen to fifteen minutes then
she died of asphyxiation. Also in 2005, an Alzheimer's patient
was hospitalized and within 24 hours after she was restrained,
was found dead related to an accidental asphyxiation (Regan,
et al., 2006).
The use of restraint in the psychiatric setting supports putting
restrictions on such policy and a program on how to deal with
uncontrollable behavior and as a result decrease in the number
of restrained patients.
Physicians, nurses, patients, other patients, and their families
are concerned about this policy; the nurse who deals with
psychiatric patients has high skill and knowledge to assess
and observe patients over 24 hours, such nurses have expert
power. The physician is the only person who has legitimate
power to get a restraining order. Regan et al. (2006) found
that other patients and their families often view patient
restraints negatively and as traumatic events there for must
be information about the indication of restraint for patients
with uncontrollable behavior so they have referent power.
Because the patient cannot refuse restraint then he/she has
no power.
Step Two: Establishing Evaluation
and Implementation Criteria
Title: Uncontrolled behavior and restraints policy
Purpose: To identify how, when, and by whom restraints
are applied.
The goal of policy is to assist patients in controlling behavior
and preventing physical injury to the patient, other patients,
visitors, and health care team.
The major desirable outcomes of behavior and restraints policy
are
A) Control patients' behavior such as anger, aggressions,
agitation.
B) Prevent harm to self and harm to healthcare team.
C) Decrease incidence of restraint use.
The undesirable outcomes that may result from this policy
are
A) Injury of patients and healthcare providers.
B) Psychological effects to patient, other patients,
family and visitors.
C) High cost effectiveness to the organization.
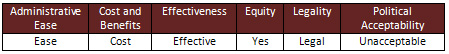
After evaluating the uncontrolled behavior and restraints
policy in National Center for Mental Health in Jordan in terms
of administrative ease, costs and benefit, effectiveness,
equity, legality, and political acceptability it was found
that:
A) Administrative ease: ease of applying the procedure
by healthcare provider, ease to restrain patient and ease
to understanding of instruction by health care team.
B) Cost and benefit: costly; needs restraint team consisting
of four to five staff during shift to apply procedure, need
training program for staff, time consuming (the patient must
be checked every fifteen minutes) and need separate room for
patient. However, the benefits of this policy is it uses the
same equipment for all patients and uses little equipment
for patients.
C) Effectiveness: it is effective by preventing self
harm and harm to health care team, controlling patient behavior
such as anger, aggressiveness and agitation, and it is a clear
policy when they are dealing with the patient. However, the
patient is isolated.
D) Equity: the policy is safe for patients, nurses
and caregivers.
E) Legality: it is legal to apply the policy because
it certified by the Ministry of Health and no harm to patient.
F) Political acceptability: unaccepted regarding human
rights and human dignity.
The following table summarizes the evaluation of uncontrolled
behavior and restraints policy in National Center for Mental
Health in Jordan.
Step Three: Suggest Alternative Policies
Managing aggressive and violent behaviors has become an important
skill for all staff who work with the psychiatric patient
(Regan, et al., 2006). After searching for alternatives and
solutions instead of use of physical restraint, some alternatives
have evidence-based practices and some have not. Regarding
uncontrolled behavior and restraints policy in the national
center for mental health, it is good but needs to be expanded.
The alternatives are
A) Personal safety plan.
B) Staff visibility in the unit.
C) Staff training.
D) Chemical restraint.
Step Four: Assessment of Alternative
Policies
All alternative policies will be evaluated in terms of administrative
ease, cost and benefit, effectiveness, equity, legality and
political acceptability, which will be summarized in a table
in five steps.
A) Personal safety plan is a primary prevention because
the health care providers do it before the patient is involved
in a distressful situation. The main goal is to gather information
about the patient's response to distress and identify what
interventions will be most helpful for him/her to stay in
control. It is initiated on admission or when the patient
can participate in the planning. If the patients do not participate
in the plan, the information is taken from family, care providers,
or previous record.
This alternative is effective since it is primary prevention
and collects data before involvement in a distress situation,
it is legal to use, safe for patient and staff, accepted politically,
easy to apply and no cost for the organization.
B) Increased staff visibility in the patient's environment
rather than present in the nurses' station. It helps the staff
to identify the problems and intervene early. This strategy
needs more staff available in the unit, which means it is
costly to the organization, effective to observe distressed
patients early, safe for patient and staff, legal to use,
easy to apply, and accepted politically.
C) Staff training is important to the patients and
staff themselves; the patient has the right to be safe when
engaging in uncontrollable behavior. This alternative is effective
since it deals with patients in a scientific method, is legal
to use, easy to apply, safe for patient and staff, but high
cost to the organization.
D) Chemical restraint by use of medication to control
patient behaviors. Most often medication used in chemical
restraint is Diazepam (Valium), Lorazepam (Ativan), and Haloperidol
(Haldol). This alternative is highly effective, legal to use,
easy to apply through medication in different routes (IM,
IV) to the patient, is of cost to the organization, safe for
patient and staff, and accepted politically.
Step Five: Distinguish Among Alternative
Policies
The following table summarizes the evaluation of the possible
alternatives:
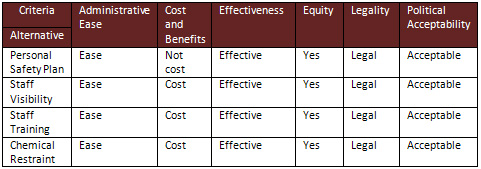
Personal safety plan is effective
since due to comprehensive assessment on admission, it is
legal, ethical, clear, safe for patient and staff, easy to
understand, evidenced based practice.
Staff visibility requires more staff available in the unit,
which means it is costly to the organization, effective to
observe distressed patients early, safe for patient and staff,
legal to use, easy to apply, is accepted politically, and
is evidenced based practice.
Staff training is effective since it deals with the patient
in a scientific method, is legal to use, easy to apply, safe
for patient and staff, high cost to organization, and evidenced
based practice. Chemical restraint is highly effective, legal
to use, easy to apply through medication, of cost to the organization,
safe for patient and staff, accepted politically, and is evidence
based practice.
Step Six: Implementation and Evaluation Plan
After evaluation of this policy and assessing all alternatives
one alternative will be chosen; many studies focus on staff
training since the staff play a major role in dealing with
these patients.
New policy: All staff on the psychiatric setting receive
a training program that can help the staff to deal with patients
and use their training instead of using restraint.
Purpose: To ensure all staff have important skills
and knowledge to deal with these patients.
A program such as crisis intervention, time management, stress
management, and development of therapeutic relationships can
help the staff to deal with these patients. Staff should receive
a training program consisting of lectures, demonstrations
and practice when starting a job.
This policy is safe for patients and staff, legal to use,
easy to apply, effective to deal with patient, but it costs
the organization.
Approval of the policy modification should be obtained from
National Center for Mental Health in Jordan, to start to implement
the modified policy, after a proper explanation and demonstration
of the missing points in this policy, which were modified
and added.
The policy evaluation will depend on the number of restraint
occurences after receiving the program.
Recommendations
• The administration for organization should develop
policy for assessment and management of uncontrollable behavior
and restraints.
• Require training program about how to deal with uncontrollable
behavior and manage it.
Summary and Conclusions
The purpose of this paper was to analyse policy used in the
psychiatric setting. I chose restraint policy since it is
a very important subject, is controversial, and a high-risk
procedure.
The use of restraint in the psychiatric setting should be
the last choice because the consequence of the procedure sometimes
is fatal. There are many alternatives that are effective,
safe to patient and staff, legal, easy to apply, and accepted
politically instead of use of physical restraint, such as
complete assessment of the patient and put into place a personal
safety plan that can help the staff to deal when the distress
situation occurs. Staff training should give the staff expert
power when dealing with the patient, as a skillful and knowledgeable
person, and there should be increased staff visibility in
the patient environment to help the staff to detect and intervene
in the distress situation early.
References
1- Cherry, B., & Jacob, S. R. (2007).Contemporary nursing:
Issues, trends, & management (5th ed.). St. Louis: Mosby.
2- Haimoqitz, S., Urff, J., & Huckshorn, K. (2006). Restraint
and seclusion- a risk management guide. Retrieved March 10,
2014, from http://www.ndrn.org/images/Documents/Issues/Restraint_and_Seclusions/
NDRN_Risk_Management_Guide.pdf
3- Lewis, M., Taylor, k., & Parks, J. (2009). Crisis prevention
management: a program to reduce the use of seclusion and restraint
in an inpatient mental health setting. Issues in mental Health
Nursing, 30, 159-164. doi: 10.1080/01612840802694171
4- Mason, D., Leavitt, J., & Chaff, M. (2007). Policy
& Politics in Nursing and Health Care (5th ed.). St. Louis:
Mosby.
5- McCue, R., Urcuyo, L., Lilu, Y., Tobias, T., & Chambers,
M. (2004). Reducing restraint use in a public psychiatric
inpatient service. Journal of Behavioral Health Services &
Research, 31(2), 217-224.
6- Regan, J., Wilhoite, K., Faheem, U., Wright, A., &
Hamer, G. (2006). The use of Restraints in psychiatric settings.
Tennessee Medicine, 41-42.
|
 |